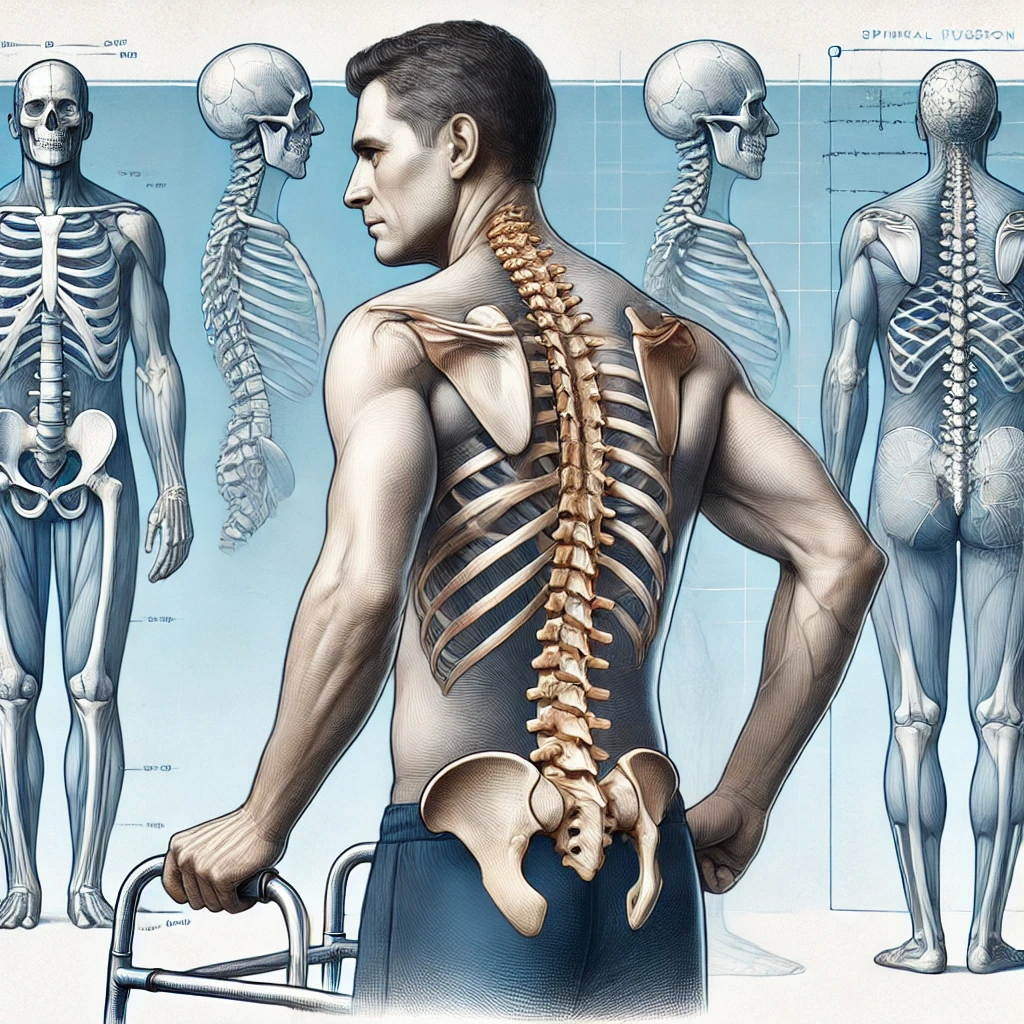
Top 10 Tips for a Successful Spinal Fusion Recovery
This article offers insights into various aspects of spinal fusion surgery, from pain management to post-operative care and recovery, based on the experiences of fellow patients.
- Find a Pain Management Specialist Before Surgery: Arrange for a pain management specialist before your surgery to ensure a seamless transition and ongoing support for pain control throughout your recovery.
- Advocate for Appropriate Pain Management: Communicate openly with your healthcare providers about your pain levels, medication needs, and any concerns you have. Don’t hesitate to seek a second opinion if necessary.
- Follow Tapering Schedules Carefully: Adhere to prescribed tapering schedules for pain medications to minimize withdrawal symptoms and reduce the risk of addiction.
- Prioritize Rest and Gradual Activity: Allow your body ample time to heal by following postoperative activity restrictions and gradually increasing activity levels as tolerated.
- Engage in Physical Therapy: Participate in a structured physical therapy program to regain strength, flexibility, and mobility. Listen to your body and avoid overexertion.
- Stay Hydrated and Maintain a Healthy Diet: Proper hydration and nutrition support the healing process and overall well-being.
- Monitor for Complications and Seek Medical Attention: Be aware of potential complications and report any new or worsening symptoms to your healthcare provider immediately.
- Utilize Non-Pharmacological Pain Management Techniques: Explore alternative pain relief methods like heat/ice therapy, massage, meditation, or TENS units.
- Build a Strong Support System: Surround yourself with supportive family and friends who can provide emotional and practical assistance during your recovery.
- Stay Positive and Patient: Recovery from spinal fusion surgery takes time. Be patient with yourself, focus on progress, and celebrate small milestones along the way.
Pain Management
Finding a pain management specialist before your surgery is a crucial step in your recovery journey. While hospitals provide pain medication after discharge, a longer-term plan is necessary. Your surgeon will monitor your recovery, but many surgical offices are hesitant to manage pain medications long-term.
- Arrange for a pain specialist beforehand to ensure a smooth transition and adequate pain control throughout your recovery.
- Pain medication is essential for surgical recovery, and appropriate pain management leads to positive outcomes and improved lives. While addiction is a possible complication, the risk is far outweighed by the benefits of pain relief during major surgery and recovery. Undergoing such procedures without adequate pain relief is far more detrimental.
The current trend of tapering off pain medication too quickly after surgery can actually increase the risk of addiction. This is because patients may aggressively consume their limited supply, leading to premature depletion and intense pain. A more effective approach is to start with a higher initial dosage that gradually decreases as the patient heals. This method prevents premature depletion, reduces pain, and mitigates the risk of addiction.
- Opioids like oxycodone should be used sparingly and short-term (maximum two weeks) due to their high addiction potential. Hydrocodone can be used for the bulk of treatment and tapering for a maximum of one year. Not tapering off opioids properly can lead to addiction.
- The Butrans patch is considered the least addictive option for chronic pain management. It is important to create a taper calendar in advance to ensure a gradual reduction in medication and minimize withdrawal symptoms.
- It is important to note that NSAIDs, while effective for pain relief, can be harmful to your kidneys, and Tylenol can damage your liver. Concerns about the impact of NSAIDs and low-dose aspirin on bone healing are valid. These medications inhibit the enzyme cyclooxygenase (COX), which plays a role in both inflammation and bone healing. This inhibition can potentially interfere with the bone healing process, particularly crucial in the first 6 to 12 months following spinal fusion surgery.
Open communication with your healthcare providers is essential throughout your pain management journey. Share your medical history, including previous treatments and their effectiveness, with your new pain management specialist. Be prepared to discuss your surgical history, pain medication use, and any side effects experienced. Actively participate in discussions about your pain management plan and ensure your concerns are addressed.
- If you feel your pain management needs are not being met, or if you have concerns about the proposed treatment plan, seeking a second opinion from another qualified pain management specialist is appropriate. Connecting with patient advocacy groups can also provide resources and support in finding specialists who understand your specific needs.
- Remember, you are your best advocate. Don’t hesitate to seek additional support or opinions when needed.
Post-Operative Care and Recovery
The intensity of postoperative pain is directly related to the number of vertebrae involved in the surgery. Peripheral and central sensitization also contribute to increased pain. However, the location of the surgery (cervical, thoracic, or lumbar spine) does not affect the pain severity.Postoperative pain is temporary and gradually improves over time, making it more manageable with medical therapy compared to chronic pain. It’s crucial to work with a pain management specialist who understands post-surgical pain and can create a personalized plan.
- Butrans (buprenorphine) is a potent opioid medication for long-term pain management that can be started effectively only with a micro-dosing strategy. This strategy involves starting with a low dose and gradually increasing it as needed to avoid withdrawal symptoms and maintain pain relief. This method is particularly helpful when transitioning from another opioid medication. Buprenorphine acts as a partial agonist, binding to opioid receptors but producing a weaker effect than full agonists like morphine or oxycodone. This characteristic makes it potentially safer for long-term pain management. However, like all opioids, it requires careful management and monitoring by a healthcare professional.
- Narco or Codeine is an opioid medication considered to be on the lower end of the potency scale, and is the best option to manage the pain effectively while minimizing the addictive potential of opioids. From jump know your tapering strategy and stay ahead.
After lumbar spinal fusion, the most severe pain typically subsides after four weeks. Patients may continue to experience some pain for three to six months, but physical therapy and healthy lifestyle habits can help manage it. Some people want to taper off and be opioid free, others plan to have pain medications the rest of their life.
Recovery Timeline and Activities
Spinal fusion surgery permanently fuses the targeted vertebrae and eliminates motion at the affected segment. This results in permanent restrictions on mobility, including an inability to twist, bend, and lift heavy objects.
- The initial three months after surgery are crucial for rest and building strength. Avoid bending, lifting, or twisting during the first four weeks and gradually increase light daily activities like walking.
- Physical therapy plays a vital role in rebuilding strength and regaining mobility. Most patients can return to their typical activities but may need to modify certain movements or avoid strenuous activities.
- It is important to listen to your body and avoid overexertion, especially in the early stages of recovery. Soreness and discomfort after physical therapy sessions are normal, indicating that your muscles are working and getting stronger.
- The DonJoy back brace is commonly used for spinal stabilization after surgery. Frequent short walks, ergonomic setup at your desk, and maintaining good posture are essential for a comfortable recovery.
Recovery from major surgery takes time and patience.
- After lumbar spinal fusion, most patients can go home within 2 to 4 days, provided they have assistance at home. The first few weeks will involve limited activity and a focus on rest.
- Around 3 to 6 months post-surgery, you should feel much better, with only intermittent fatigue. By the six-month mark, fatigue should be resolved entirely.
- Complete recovery from spinal fusion surgery usually takes up to 8 months, with bone continuing to evolve for 12 to 18 months.
Revision Surgery Considerations
If complications arise after the initial spinal fusion, a revision surgery may be necessary.
- Extending the fusion to more vertebrae can help stabilize the spine and reduce pain. However, it also further reduces mobility and can increase surgical risks, including blood loss, infection, and longer recovery times. It is important to have a detailed discussion with your surgeon about the potential benefits and risks of revision surgery and consider seeking a second opinion.
- Limiting the new incision to the area that needs revision can minimize surgical trauma and preserve healing tissues, especially if the previous surgery was recent. This targeted approach allows the surgeon to focus on the specific area requiring attention. However, it is important to discuss any concerns or questions about the surgical approach with your surgeon.
- Managing pain after revision surgery is crucial. Discuss your pain management plan with your surgeon and anesthesiologist and ensure it includes a combination of medications, possibly including nerve blocks or epidural analgesia. Effective pain control is essential for a comfortable recovery.
- Communicate with your surgical team about your current pain management regimen, especially if you are using a Butrans patch. They will need to adjust your pain management plan accordingly.
Preparing mentally and physically for revision surgery is important. Educate yourself about the procedure and recovery process, ask your surgeon any questions you have, and consider talking to a therapist or counselor for support. Engage in positive activities like hobbies or spending time with loved ones to reduce anxiety.
- Before revision surgery, have a detailed conversation with your surgeon and anesthesiologist about your previous experience with pain management. Emphasize the need for a robust pain management plan in the immediate postoperative period.
- Returning to activities like cycling after spine surgery is possible, but it’s crucial to prioritize safety and follow medical advice. A comprehensive physical therapy program will help regain strength, flexibility, and balance necessary for cycling.
- Gradual reintroduction to physical activity is key, and it’s important to make any necessary adjustments to your equipment and cycling habits. Always consult your healthcare team before resuming any physical activity to ensure it is safe for you.
If you experience severe, unrelenting pain after surgery that requires high doses of pain medication, contact your surgeon or pain management specialist immediately.
- Keep a detailed record of your pain levels, medication usage, and any other symptoms to share with your healthcare team.
- Seek immediate medical attention if you experience new or worsening symptoms, such as loss of bowel or bladder control, significant weakness, or numbness in your legs, as these could be signs of a more serious condition.
- Engage with your support network and consider speaking with a mental health professional to help manage the emotional toll of chronic pain.
Muscle Pain and Peripheral Neuropathy
It is normal to experience soreness and pain after spinal fusion surgery. Pain is typically caused by surgical trauma, the healing process, nerve healing, scar tissue formation, and the spine’s adjustment to its new configuration.
- To manage muscle pain after spinal fusion surgery, your doctor may recommend medications, muscle relaxants, heat therapy, and physical therapy. Keep your healthcare team informed about your pain levels and any changes in symptoms.
- Leg, ankle, and feet swelling, along with loss of motor control after spinal fusion surgery, could be caused by dependent edema, deep vein thrombosis (DVT), heterotopic ossification, nerve compression, or lymphedema.
To address these issues, perform regular leg movements, elevate your legs when resting, use compression stockings as prescribed, stay hydrated, and monitor for any signs of complications. It’s crucial to consult with your surgeon or healthcare provider for a proper evaluation and treatment plan.
Also see Comprehensive Spine Surgery Guide