Frustrations of Post-Surgical Care Amidst the Opioid Crisis
Navigating post-surgical care in the current climate of the opioid crisis has become an excruciatingly challenging experience. Recently, I underwent a major spine surgery involving both Anterior Lumbar Interbody Fusion (ALIF) from L3 to S1 and Posterior Spinal Fusion (PSF) from T10 to the pelvis. While the surgery’s outcomes are promising, the extent of muscular and tissue trauma incurred is significant.
The intensity of this surgery is immense, arguably one of the most invasive procedures one can endure. However, in the midst of today’s opioid crisis, the approach to managing post-surgical pain feels archaic, almost as if we’ve regressed to medieval times where pain endurance was the only option. Pain management, which is crucial for both recovery and quality of life during the healing process, seems to be grossly overlooked.
Currently, pain medication prescriptions are heavily regulated, allowing only a five-day supply at a time. Compounding this issue is the requirement of a two-day processing period for refills. This system virtually guarantees that patients, myself included, will run out of pain medication every four days. Such gaps in pain management are not just uncomfortable; they are unbearable and inhumane, considering the level of pain associated with such extensive surgeries.
Moreover, this inadequate pain control significantly hampers the recovery process. The overwhelming pain from the surgical trauma masks any real sense of healing progress. It becomes challenging, if not impossible, to gauge the body’s healing when the focus is entirely consumed by managing relentless pain. This situation raises serious concerns about the effectiveness of current post-surgical care protocols, especially in the context of major surgeries like mine.
It’s imperative to find a balance that addresses the opioid crisis without neglecting the legitimate needs of patients recovering from major surgeries. Pain management should be a fundamental component of post-operative care, and the current system feels like it falls short of addressing this critical need.
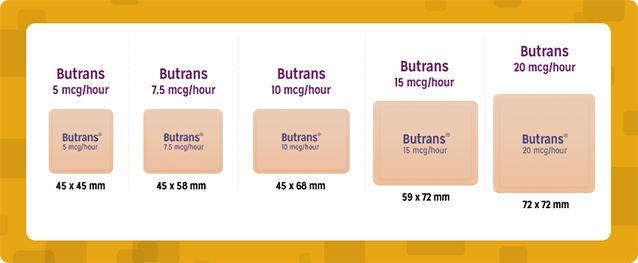
I have found the Butrans patch works best, has the most pain relief, is applied only once a week, and has the least side effects.
- Butrans, which contains buprenorphine, is a medication used for managing pain. It’s part of a class of drugs known as opioid analgesics. The patch is applied to the skin and provides a steady release of medication over a seven-day period, which can be convenient and beneficial for those who need consistent pain management.
- It’s important to remember that individual responses to pain medications can vary significantly. What works well for one person might not be as effective for another. Additionally, opioids, including Butrans, have risks and potential side effects, such as dependency, respiratory depression, and others. It’s crucial to use them under the guidance of a healthcare professional who can monitor their effectiveness and safety.
- I encourage anyone to consult with their healthcare provider to determine the best pain management strategy for their specific needs and health profile.
You don’t get a “high feeling” from the Butrans patch, just pain relief!

