The VA Community Care Program is a system established by the Department of Veterans Affairs (VA) to provide eligible veterans access to healthcare services from private providers outside the VA healthcare system. It was created to expand access to timely care, especially when VA facilities are unable to meet veterans’ needs due to distance, availability, or specialized care requirements.
Here’s an overview of how the program works:
Key Features of the VA Community Care Program
-
Eligibility Criteria:
Veterans may qualify for community care if:
-
- The VA cannot provide the care they need.
- They live too far from a VA facility (typically 40 miles or more).
- Wait times for VA care exceed certain standards (e.g., 20 days for primary care, 28 days for specialty care).
- They need a specific type of care not offered at VA facilities.
- It is in the veteran’s best interest, as determined by their VA healthcare provider.
-
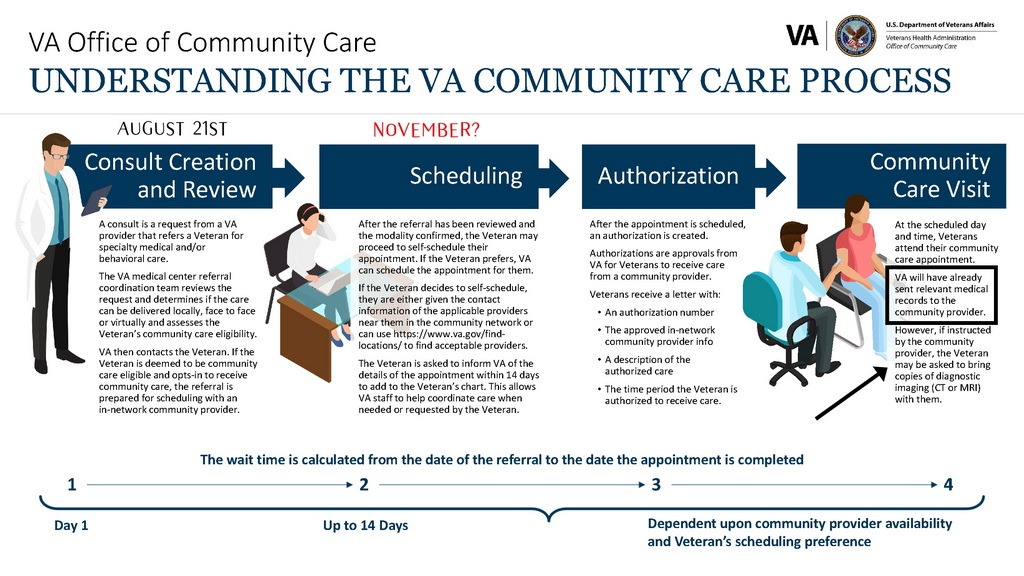
Referral Process:
Veterans must first receive approval and a referral from the VA to access care through the program. The VA coordinates with community providers to schedule appointments and manage medical records. -
Coordination of Care:
The VA acts as the primary coordinator, responsible for managing authorizations, sharing records, and ensuring the continuity of care between VA facilities and private providers. -
Costs:
Veterans generally pay the same copayments for community care as they would for VA-provided care. The VA reimburses community providers directly for authorized services.
Challenges and Criticisms
While the VA Community Care Program aims to improve access and reduce delays, it faces several challenges:
-
Administrative Inefficiencies:
-
- Delayed authorizations and poor coordination between the VA and community providers can lead to gaps in care.
- Veterans often report difficulty navigating the program and getting timely appointments.
-
Continuity of Care Issues:
-
- Some community providers fail to send records back to the VA, leaving gaps in the veteran’s medical history.
- The “fire-and-forget” referral model has led to veterans being abandoned by private providers after mistakes or disputes.
-
Accountability Gaps:
-
- Community providers are not held to the same oversight standards as VA facilities, leading to inconsistencies in care quality.
-
Costs and Sustainability:
-
- The program is expensive to administer, raising questions about its long-term financial sustainability and potential strain on VA resources.
The VA Presidential Hotline 855-948-2311
Pledged by President Donald J. Trump as part of his administration’s commitment to reforming the U.S. Department of Veterans, the hotline, 855-948-2311, serves Veterans, their families, caregivers and survivors by giving them a direct, nonemergency, contact line available 24 hours a day, 365 days a year with agents — the majority of whom are Veterans or from a Veteran family — who are trained to address general and common VA inquiries.
This hotline will get your issue addressed!
Key Issues with the VA Community Care Program
The VA Community Care Program offers veterans access to private healthcare providers when VA facilities are unable to meet their needs. However, significant challenges and systemic issues have made many veterans hesitant to use the program. These fears stem from administrative failures, gaps in care coordination, and personal experiences that undermine trust in the program.
1. Administrative Inefficiencies
-
- Delayed Referrals and Approvals: Veterans often face long waits for referral approvals and appointment scheduling, defeating the program’s purpose of providing timely care.
- Poor Communication: The VA and community providers frequently fail to coordinate effectively, leaving veterans in the dark about the status of their care.
- Billing Confusion: Miscommunication between the VA and private providers sometimes leads to veterans being billed directly for services, causing financial stress and frustration.
2. Lack of Oversight
-
- Quality of Care: Community providers are not held to the same oversight and accountability standards as VA facilities, leading to inconsistent care.
- Records Gaps: Many community providers fail to send medical records back to the VA, resulting in fragmented care and incomplete medical histories.
3. Continuity of Care Problems
-
- “Fire-and-Forget” Referrals: After a referral is made, the VA often does not follow up with veterans or providers, leaving veterans without guidance or support.
- Abandoned Care: Some private providers terminate care abruptly after errors or disputes, leaving veterans without treatment or access to necessary follow-ups.
4. Cost and Financial Uncertainty
-
- While the VA is supposed to cover the costs of authorized care, administrative errors sometimes result in veterans being sent to collections for unpaid bills that were not their responsibility.
5. Geographic and Accessibility Challenges
-
- Limited Provider Networks: Not all areas have a robust network of community providers, especially rural regions, making it difficult for some veterans to find care.
- Travel Burdens: Veterans may still need to travel significant distances to access care, despite the program’s intention to reduce travel requirements.
6. Accountability Gaps
-
- No Clear Responsibility: Veterans caught between the VA and community providers often find it unclear who is responsible when issues arise, leading to frustration and delays in resolving problems.
- Medical Errors and Negligence: Some veterans report experiencing substandard care or errors from community providers, with no clear mechanism for accountability or recourse.
7. Mental Health Stigma
-
- Veterans with mental health conditions often find it especially challenging to navigate the complexities of the program, leading to worsened mental health outcomes and reluctance to seek care.
Why Veterans Are Afraid to Use the Program
1. Fear of Abandonment
-
- Many veterans worry they will lose access to care entirely if a community provider refuses to continue treatment, as VA facilities may not step in promptly to fill the gap.
2. Distrust in the System
-
- Veterans who have faced bureaucratic hurdles or experienced negligence in the VA system fear the program will only exacerbate these issues, particularly given the lack of direct oversight of private providers.
3. Financial Anxiety
-
- Stories of veterans being wrongly billed or sent to collections create a pervasive fear of financial hardship, discouraging many from seeking care through the program.
4. Fear of Fragmented Care
-
- Veterans worry about incomplete medical records and poor communication between the VA and community providers, leading to disjointed or inappropriate treatment.
5. Bad Past Experiences
-
- Veterans who have experienced delays, errors, or substandard care in the Community Care Program are often reluctant to use it again, preferring to endure longer wait times at VA facilities rather than risk repeating their negative experiences.
6. Concerns About Accountability
-
- Veterans are hesitant to use a program where it’s unclear who will take responsibility if something goes wrong, leaving them vulnerable in cases of medical negligence or administrative errors.
How These Issues Affect Veterans
These challenges create a cycle of mistrust and fear, discouraging veterans from accessing the care they need. Veterans often feel they must navigate the program alone, acting as their own advocates to ensure appointments are scheduled, records are shared, and bills are resolved. For those already dealing with serious health conditions, this added burden can feel overwhelming.
The VA Community Care Program was designed to address gaps in VA healthcare access, but its execution has left many veterans feeling unsupported, anxious, and afraid to use it. Addressing these issues requires systemic reform, including better oversight, improved communication, and streamlined processes to restore veterans’ confidence in the program. Until then, veterans must remain vigilant, keeping detailed records and advocating for themselves in a system that often feels stacked against them.
Benefits for Veterans
Despite these challenges, the program provides several important benefits:
- Improved Access: Veterans in rural areas or with complex medical needs can access care closer to home or through specialists not available at VA facilities.
- Choice of Provider: Veterans have more options for their care, allowing them to seek providers they trust or who specialize in their conditions.
- Reduced Wait Times: When functioning well, the program helps alleviate delays in accessing VA care.
Program Evolution
The VA Community Care Program was enhanced by the MISSION Act of 2018, which replaced the earlier Veterans Choice Program. The MISSION Act streamlined eligibility criteria, expanded the network of community providers, and aimed to improve care coordination.
Conclusion
The VA Community Care Program is a critical lifeline for veterans requiring timely and specialized healthcare. However, its effectiveness depends heavily on proper coordination, transparency, and accountability. Veterans using the program should be proactive in managing their care, maintaining records, and following up with both VA and community providers to ensure they receive the best possible outcomes.