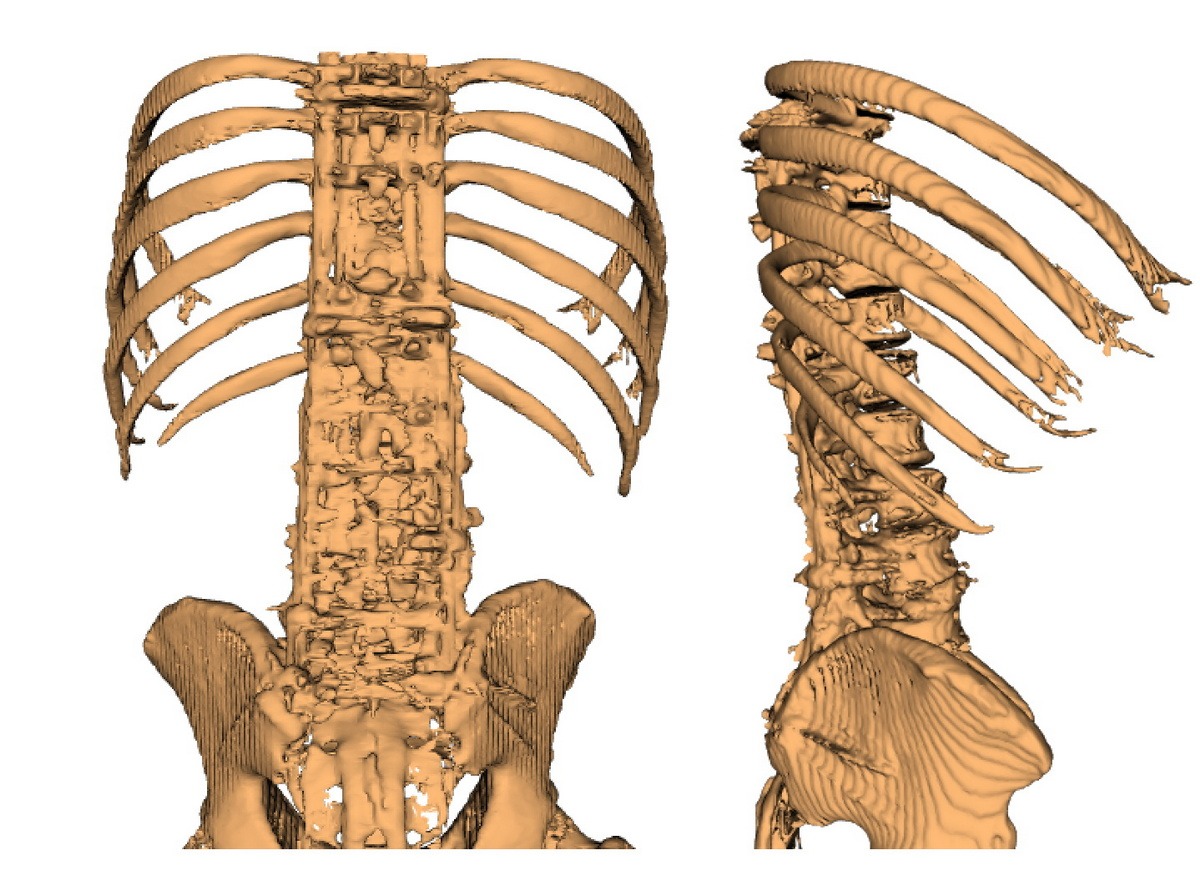
These 3D spinal models illustrate the story of how a hidden surgical error and delayed treatment to revise it – transformed a correctable spinal condition into five years of disability, before a team at Baylor Medical Center came into the picture – operated for over 12 hours – and built me a new spine.
- The progression begins in April 2021, showing my spine with normal lumbar lordosis (the natural inward curve of the lower back) but a specific problem – retrolisthesis at L3-L4, where one vertebra had slipped backward relative to the one below it. This condition warranted a targeted fusion from L2 to L4.
- Instead, surgery was performed at the wrong levels (L1-L3), leaving the problematic L3-L4 segment untreated. The October 2021 model reveals the consequences: loss of lordosis had already begun, and the untreated retrolisthesis was worsening.
- By October 2023, the progression is stark – the model shows classic flatback syndrome, where the spine has lost its natural curves, forcing me to bend forward just to stand.
- The final model from November 2024 demonstrates the extensive reconstruction required to correct this preventable progression.
Thank God the Baylor surgery restored my sagittal balance, allowing me to stand upright and walk again. I now have a spine that’s super sturdy.
3D Model 2024
Understanding spinal biomechanics through these models makes clear how the wrong-level surgery and untreated complications created a cascade of structural problems. What began as a correctable condition at a single spinal segment ultimately required fusion of nearly the entire spine – an outcome that proper surgical planning and timely intervention could have prevented.
A Personal Note to Those Considering Spine Surgery:
Your spine is too important to leave entirely in someone else’s hands. As someone who learned this lesson the hard way, I strongly encourage you to be an active participant in your surgical care – especially when navigating complex systems like VA community care. Get independent surgical opinions both before and after your procedure. More importantly, take advantage of modern technology: having your CT scans converted to 3D models can help you understand your condition and surgical plan in concrete terms.
These visual tools aren’t just educational – they’re protective. When I finally saw 3D models of my spine’s progression, the surgical error and its consequences became immediately clear. Had I had these models from the start, I could have identified and addressed complications before they led to disability. While most surgeons are dedicated professionals, healthcare systems don’t always prioritize transparency when complications arise. Having your own clear understanding of your spinal anatomy and surgical plan creates an essential layer of accountability.