I never imagined a routine spine surgery would become the catalyst for years of suffering and a fight for medical justice. In August 2021, I trusted my surgeon and the VA healthcare system to fix a relatively straightforward spinal problem. Instead, I woke up to what would become a nightmare – though I wouldn’t understand the full extent of it for months to come.
The first signs that something was wrong came through intense, unusual pain that didn’t match the expected post-surgical recovery. By October 2021, VA imaging revealed the devastating truth: the surgeon had operated on the wrong spinal levels, left hardware loose, and placed screws that breached my spinal canal. But rather than immediately addressing these clear surgical errors, I faced a wall of institutional silence. For two years, I watched helplessly as my condition deteriorated, my mobility decreased, and my pain intensified.
Despite regularly showing up for appointments, despite CT scans clearly showing the progressive damage, despite my increasingly desperate reports of severe pain and declining function, I received nothing but pain medications and palliative care. The system seemed designed to protect the surgeon rather than help the patient. I felt trapped in a medical maze where every turn led to another dead end.
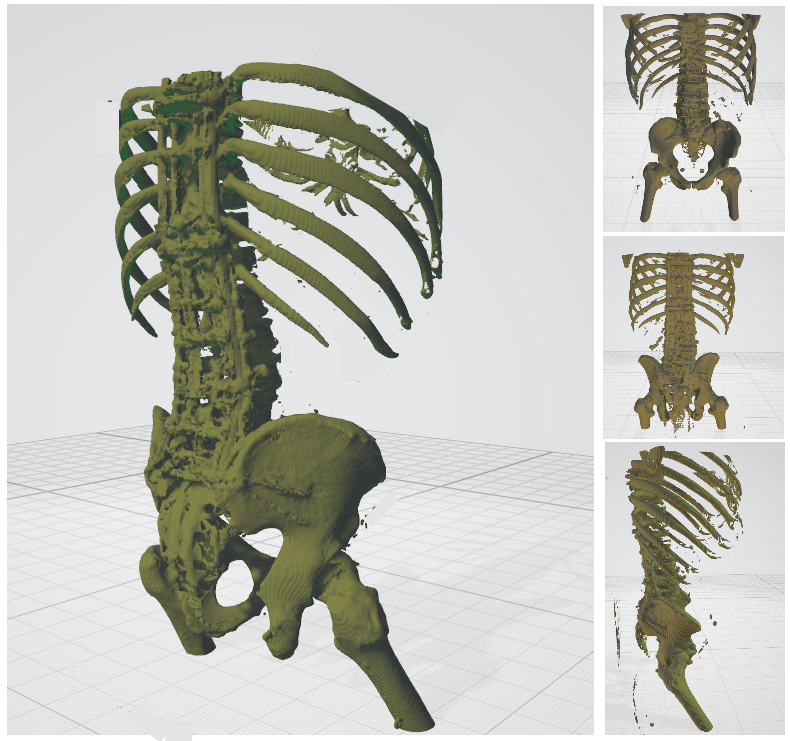
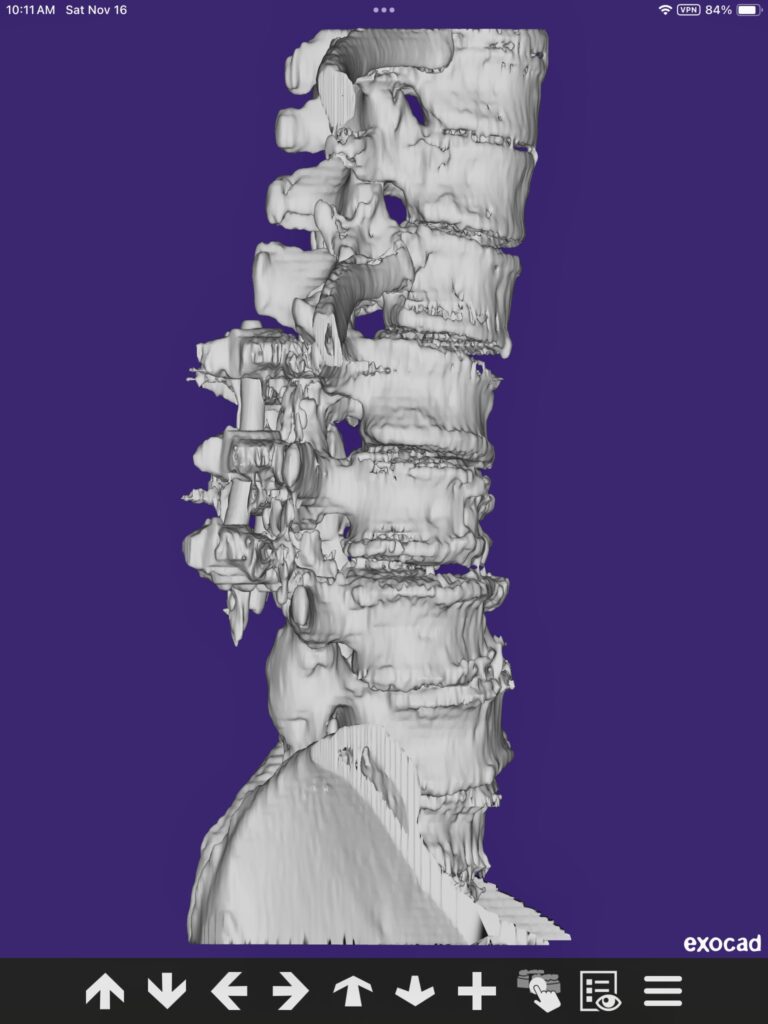
It wasn’t until January 2024, when I finally made my way to Baylor Scott & White Medical Center, that I found surgeons willing to acknowledge and address the full scope of the damage. Their operative notes tell the technical story – destroyed pedicles at L1 and L3, severe sagittal imbalance, and spinal instability requiring extensive reconstruction from T4 to my pelvis. But those clinical terms can’t capture the human cost: two years of preventable suffering, permanent damage to my spine, and a profound loss of the life I once knew.
My story illustrates a troubling reality that too many patients face: the near-impossible task of seeking accountability when surgical errors occur. While I understand that surgeons need reasonable protections to practice their complex profession, the current system too often leaves patients like me bearing the full burden of their mistakes – physically, emotionally, and financially.
The most frustrating part? This isn’t an isolated incident. As I’ve navigated this medical maze, I’ve discovered countless others with similar stories – patients whose surgical errors were buried under layers of institutional protection, their suffering dismissed or minimized. It’s a systemic problem that demands attention and reform, not just for my sake, but for every patient who follows.
The Evidence
See for yourselves:
 |
 |
| Before | After |
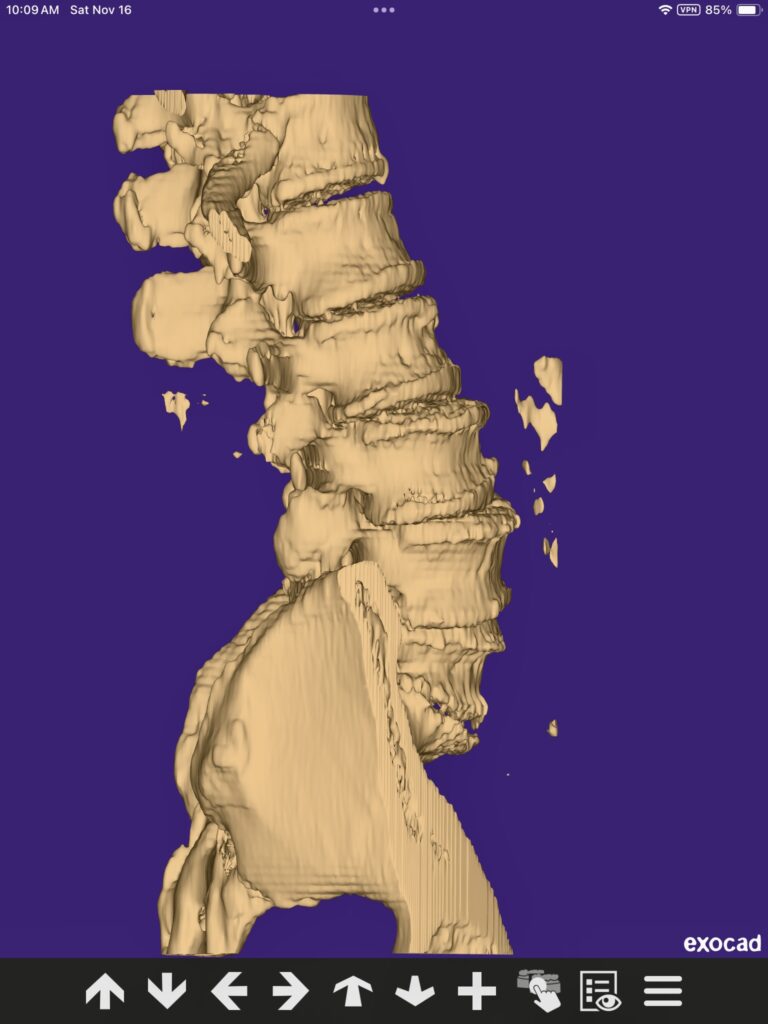
My spine after they fused the wrong vertebrea, the loss of lordosis curve is clearly visible on the right
A more detailed narrative of what happened:
The problems with my spine trace back to a critical surgical error in August 2021. While the surgical plan called for fusion at L2-L4, the surgeon instead fused L1-L3, completely missing the L3-L4 level that was causing most of my problems. This mistake started a chain reaction of complications that would get progressively worse over the next two years.
The incorrect fusion created two major problems for me. Not only did fusing L1-L3 put extra stress on my already damaged L3-L4 level, but CT scans in October 2021 showed the surgical hardware was failing, with loose screws that would eventually break through the spinal canal at L1 and L3. When I finally had corrective surgery at Baylor in January 2024, they found these loose screws had actually destroyed the bone structure in those areas of my vertebrae.
During those two years without proper treatment, my spine gradually lost its natural lower back curve. This happened because several things were working against me at once: my untreated L3-L4 level kept getting worse under abnormal pressure, the loose hardware wasn’t holding my spine in proper alignment, and the incorrect fusion levels had disrupted my spine’s natural mechanics. When I finally saw Dr. Rizkalla at Baylor in November 2023, he confirmed I had developed flatback syndrome – my spine had lost its normal curvature, causing my trunk to tilt forward.
My records show how things kept getting worse. By September 2023, I was in such bad shape that the VA had to give me a wheelchair because I could barely walk. When I finally had corrective surgery at Baylor in January 2024, they found so much damage that they had to do an extensive fusion from T10 to my pelvis. They later had to extend this even further to T4 to restore proper alignment – a much bigger surgery than I would have needed if the original error had been fixed promptly.
The Final Outcome in 2024
The skilled surgical team at Baylor Scott & White Spine and Scoliosis Center successfully restored my ability to walk and significantly reduced my pain, but the extensive nature of the corrective surgery has left me with some limitations. The procedure they had to perform – a fusion extending from T4 all the way to my pelvis – was necessary to correct the severe spinal deformity that developed during those two years without proper treatment. This extensive fusion successfully restored my spinal alignment and relieved much of my pain, best of all, I can stand and walk and travel and work again!
Looking back, I can see how that initial surgical error, combined with two years without proper treatment, led to the complete breakdown of my spine’s natural structure. This forced me to undergo far more extensive surgery than I would have needed if I’d received proper care from the beginning.
This isn’t a story of simple misfortune or isolated human error – it’s a documented pattern of negligence where multiple providers failed to address clear evidence of surgical complications, leading to preventable suffering and permanent disability. The medical record shows not just what went wrong, but precisely when and how it could have been prevented through standard medical intervention.