Claimant: Michael A. Stuart Date of Birth: January 13, 1959 Claim Date: November 27, 2024 Claim Type: Federal Tort Claims Act (Standard Form 95) for personal injury/wrongful death, specifically an “1151 claim” related to VA negligence. Federal Agency: Department of Veterans Affairs, Office of General Counsel, Torts Law Group
Executive Summary
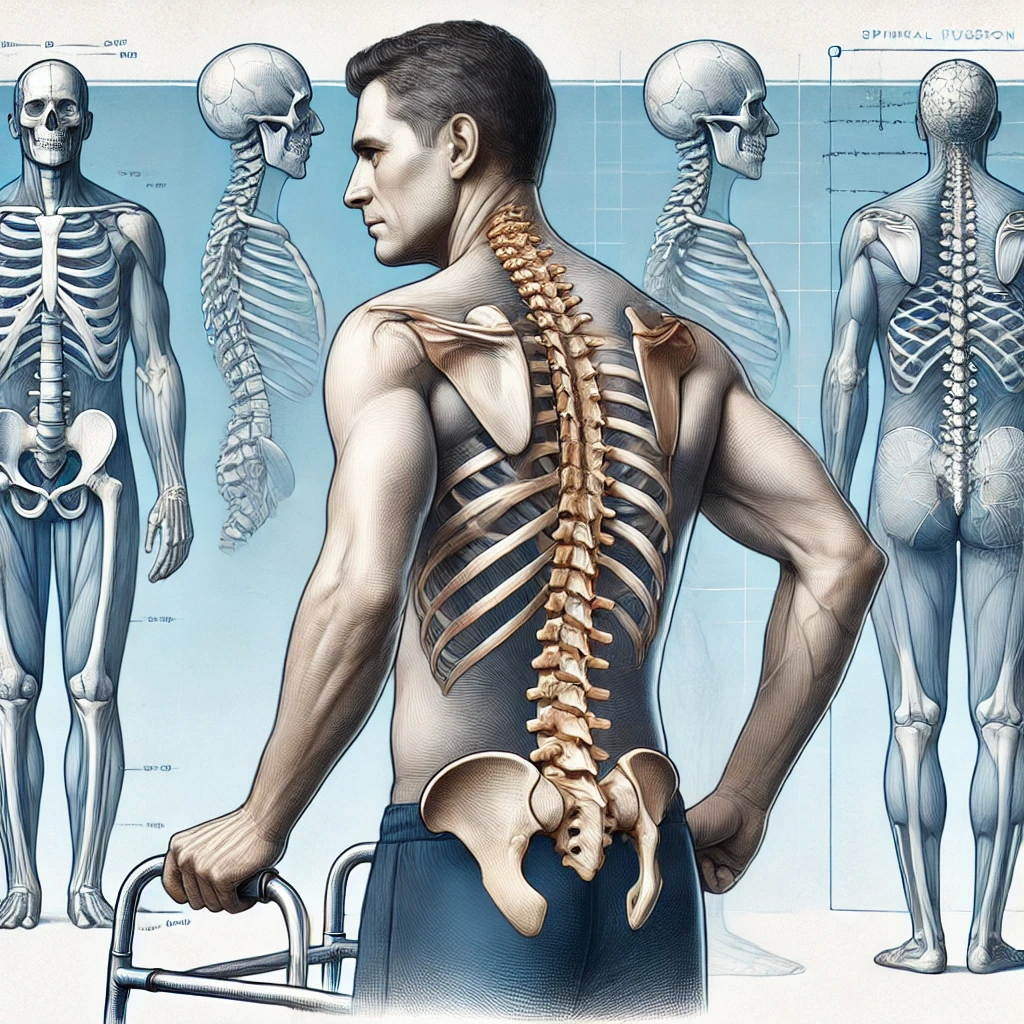
Michael A. Stuart is filing a detailed claim alleging severe and permanent spinal disability, specifically “permanent ankylosis of the spine requiring fusion from T4 to pelvis,” directly resulting from negligent care by the Dallas VA Medical Center. The negligence stems from a two-year delay (October 2021 to October 2023) in addressing documented loose pedicle screws and hardware failure following an August 2021 spinal fusion surgery performed through a VA Community Care program. This delay, despite Stuart’s persistent complaints and clear imaging evidence, led to preventable damage, the development of “flat back syndrome,” and ultimately necessitated extensive corrective surgery by Baylor Medical Center in January 2024. This has left Stuart with profound physical limitations, chronic pain, and significant impact on his quality of life and ability to work, rendering him dependent on others for support. He is seeking a 100% VA disability rating.
Key Themes and Facts
I. Initial Spinal Issues and VA Community Care Surgery (2019-2021)
- April 2019: Stuart was involved in a serious car accident (not his fault), leading to a laminectomy at the Dallas VA Hospital in July 2019.
- August 2021: A subsequent spinal fusion at L2-L4 was performed through a VA Community Care program by Dr. Kesterson.
- Allegation: Stuart later discovered that the surgeon “operated on the wrong parts of my spine” and fused L1-L3 instead of the planned L2-L4. He also alleges the surgeon “left pedicle screws loose.”
- Surgeon Abandonment: Dr. Kesterson “disappeared without addressing the issue,” leaving his practice in January 2022, and was later “sanctioned by the Texas Medical Board” for this surgery.
II. VA’s Negligent Delay and Misdiagnosis (October 2021 – October 2023)
- October 2021 CT Scan: A VA CT scan on October 30, 2021, “revealed that the surgery had failed, showing loose pedicle screws and non-union, putting my spine at risk.” Specifically, “Mild lucency is noted along the left L1 and right L3 transpedicular screws. Significant lucency is noted along the left S3 transpedicular screw.” The report also noted “Aneurysmal dilatation of common iliac arteries.”
- Patient Complaints and VA Inaction: Despite these findings and Stuart’s “persistent pleas for help,” the VA “did not take corrective surgical action for the next two years.”
- Stuart repeatedly contacted VA staff (PCP, Neurosurgery, Community Care) about “unusual pain,” “severe-severe pain,” “inability to walk or stand but briefly,” “gross swelling in my feet and ankles,” “shortness of breath,” and “weird numbness in buttocks groin” following the 2021 surgery.
- VA staff, including Neurosurgery Nurse Practitioner Diana Medina-Cattarin and PCP Dr. Shehla Naz, were made aware of these complaints and the October 2021 CT findings of lucency.
- Community care providers reportedly “declined the case due to the previous surgical failure and abandonment by the surgeon.”
- September 2021: The VA provided Stuart with a wheelchair, indirectly acknowledging his “complete loss of mobility.”
- June 2023 CT Scan: This VA CT scan “failed to mention the ’emergency spinal conditions’ that the Baylor team later identified in October 2023.” While it noted “Evidence of prior surgery with fusion in the lumbar spine seen from L1 through L3 with the bilateral pedicle screws and posterior stabilizing interconnecting bars. Hardware is in good position,” and “Moderate to severe scoliosis of the lumbar spine,” it did not explicitly mention sagittal alignment issues, flat back syndrome, or pedicle screw lucency, stating “the hardware is noted to be in good position.” This contradicts Stuart’s prior CT findings and later Baylor diagnosis.
- Failed Referrals: Multiple attempts to get a referral to community care neurosurgery (e.g., to Dr. Cattorini or UTSW) were met with delays and rejections from providers or the community care system itself, often stating “no referral for community care. Please contact your PCP.”
III. Baylor Medical Center Intervention and Corrective Surgery (October 2023 – January 2024)
- October 2023: “Frustrated, in agonizing pain, and in a wheelchair provided by the VA,” Stuart hired Baylor Medical Center to investigate.
- Baylor Diagnosis: Baylor immediately diagnosed “the failed surgery and the damage to my spine and that a new disabling condition developed called flat back syndrome.” They also identified “loss of sagittal alignment (flat back syndrome), pedicle screw lucency, non-union, and physical damage to the L1 and L3 vertebrae.”
- VA Acknowledgment: The Dallas VA “effectively admitted their negligence by providing secondary funding for Baylor Medical Center,” covering the cost of the corrective surgery.
- January 2024 Corrective Surgery: Baylor performed “the most extensive spinal fusion from T4 to pelvis to restore my sagittal balance, correcting the flat back syndrome.” This surgery “removed failed surgery hardware, repair the damaged spine.”
IV. Current Condition and Disability
- Permanent Ankylosis: The corrective surgery resulted in “permanent Ankylosis of the Spine,” characterized by “the permanent loss of natural movement in 15 vertebrae, severely limiting the ability to bend, twist, or perform other spinal motions.”
- Specific Disabilities: These include “ambulatory dysfunction, severe chronic pain, and permanent spinal deformity requiring extensive surgical reconstruction.”
- Profound Limitations:Loss of Spinal Flexibility: Inability to bend forward, backward, side-to-side, or twist at the fused sections (T4 to pelvis).
- Mobility Issues: Difficulty walking (gait altered, painful, exhausting), struggling with balance, and limited range of motion for daily activities like getting out of bed, sitting, standing, or driving.
- Difficulty with Daily Activities: Requires assistance or adaptive equipment for self-care (shoes, socks, pants) and household chores (cleaning, lifting, grocery shopping).
- Chronic Pain & Fatigue: Ongoing pain at the fusion site and other areas, leading to “extreme fatigue” due to compensation.
- Respiratory Issues: Reduced rib cage expansion, causing “difficulty taking deep breaths and causing shortness of breath, particularly during exertion.”
- Altered Posture: Rigid and upright posture, leading to further strain.
- Mental/Emotional Impact: Reduced quality of life, frustration, depression, anxiety, and social isolation.
- Financial Impact: Stuart is “physically, mentally, and financially exhausted,” living “impoverished,” and “slowly losing assets that cannot be replaced.” He anticipates losing his automobile and inability to obtain housing near family.
- Witness Testimony: Colonel Christopher S. Ceplecha (USAF ret.), Michael Stuart’s brother-in-law, attests to Michael’s decline from “epitome of vigor” to “relentless pain and debilitation,” needing a walker and having his spirit visibly affected. He highlights the “disheartening” lack of VA response.
V. VA Disability Rating Context
- Diagnostic Code 5241: Spinal fusion is rated by the VA under this code, based primarily on range of motion limitations.
- Potential 100% Rating: “Unfavorable ankylosis of the entire spine” is the maximum schedular rating (100%). A fusion from T4 to the pelvis is considered “significant surgery” and “would involve a large portion of the spine, likely resulting in significant loss of motion and functional impairment.”
- Key Factors for Rating: Range of motion, pain levels (especially during motion), functional impairment (ability to perform daily activities and work), location/extent of fusion, and secondary conditions.
- Stuart’s Claim: He believes his condition qualifies for a “100% disability rating due to the total loss of function, mobility, and the profound impact on my quality of life.”
Conclusion
Michael A. Stuart’s claim details a clear progression of medical malpractice and negligent care by the Dallas VA Medical Center and its community care providers, leading to a severely debilitating spinal condition. The documented timeline of failed surgery, ignored symptoms, delayed intervention, and subsequent extensive corrective surgery by a private institution (funded by the VA as an implicit admission of fault) forms a compelling basis for his Federal Tort Claim and request for a 100% disability rating. The medical evidence and personal accounts strongly support the assertion that his permanent ankylosis and associated disabilities are a direct result of the VA’s failures, rather than a natural progression of his initial condition.